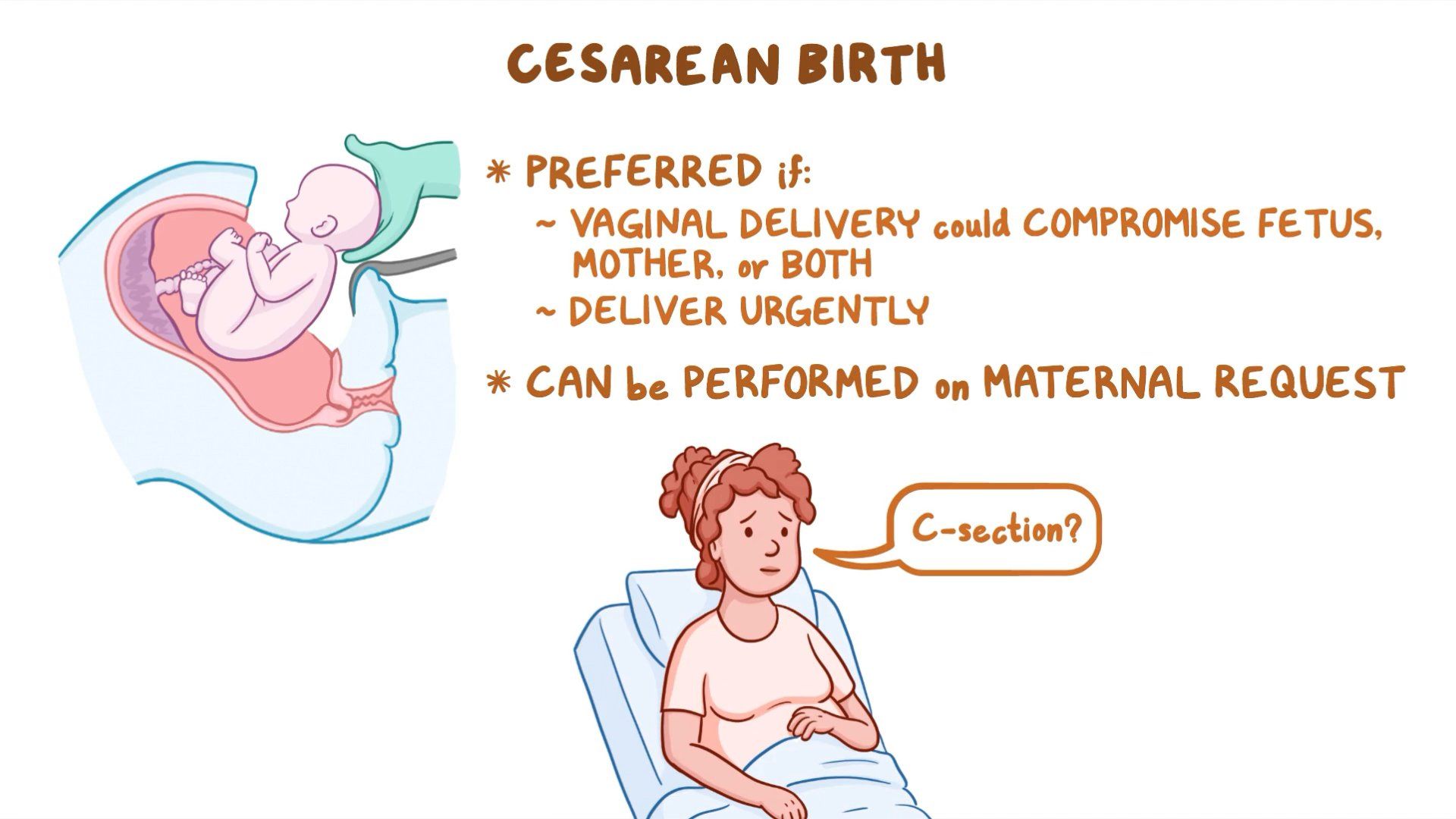
Cesarean delivery, also known as C-section, is a surgical procedure used to deliver a baby through incisions in the abdomen and uterus. This method is often employed when a vaginal delivery would pose risks to the mother or baby. Understanding the critical assessment findings during and after a cesarean delivery is essential for nurses and healthcare providers to ensure the safety and well-being of both mother and child.
This article will explore the various assessment findings that nurses must prioritize in the context of cesarean deliveries. It will cover the physiological changes that occur during the procedure, as well as the potential complications that may arise. By identifying and responding to key assessment findings, nurses can enhance patient outcomes and provide quality care. Additionally, we will discuss the importance of evidence-based practices in managing cesarean deliveries.
As the rate of cesarean deliveries continues to rise globally, understanding the associated risks and required nursing assessments becomes increasingly vital. This article aims to equip healthcare professionals with the knowledge needed to prioritize assessment findings effectively, thereby improving the overall quality of maternal and neonatal care.
Table of Contents
Biography of Cesarean Delivery
Cesarean delivery has a rich history dating back to ancient times, with its methods evolving significantly over the centuries. Initially, cesarean sections were performed only when the mother was deceased or dying, but advances in surgical techniques and anesthesia have made it a safer option for both mothers and infants.
| Term | Description |
|---|---|
| Definition | A surgical procedure to deliver a baby through incisions in the abdomen and uterus. |
| Indications | Health issues in the mother or baby, prolonged labor, or abnormal fetal position. |
| Types | Elective and emergency cesarean deliveries. |
| Risks | Infection, blood loss, and complications in future pregnancies. |
Physiological Changes During Cesarean Delivery
During a cesarean delivery, several physiological changes occur in the mother and fetus:
- Increased blood volume and altered hemodynamics due to fluid administration.
- Changes in uterine contractions and placental perfusion.
- Potential for respiratory depression in the neonate due to anesthesia.
Key Assessment Findings
Nurses must be vigilant in monitoring specific assessment findings during and after a cesarean delivery. Some of the critical findings include:
1. Vital Signs Monitoring
- Heart rate, blood pressure, and respiratory rate should be regularly monitored.
- Abnormalities may indicate complications such as hemorrhage or infection.
2. Uterine Assessment
- Assess the firmness and position of the uterus post-delivery.
- Monitoring for uterine atony is crucial, as it can lead to postpartum hemorrhage.
3. Incision Site Examination
- Inspect the surgical incision for signs of infection, such as redness, swelling, or discharge.
- Ensure that the incision is healing properly without complications.
Potential Complications of Cesarean Delivery
Several complications can arise from cesarean deliveries, and nurses should be aware of these to prioritize assessment findings effectively:
- Infection at the incision site or in the uterus.
- Hemorrhage leading to hypovolemic shock.
- Thromboembolic events such as deep vein thrombosis (DVT).
Nursing Priorities During Cesarean Delivery
To ensure optimal patient care, nurses must prioritize the following during and after cesarean delivery:
- Immediate post-operative assessment to identify complications early.
- Education for the mother regarding recovery and signs of potential complications.
- Support for breastfeeding and bonding with the newborn.
Importance of Evidence-Based Practice
Incorporating evidence-based practices into nursing care during cesarean deliveries is vital for improving patient outcomes:
- Utilizing standardized protocols for monitoring and assessment.
- Staying updated with the latest research on cesarean delivery risks and management strategies.
- Participating in continuing education programs to enhance clinical skills.
Conclusion
In conclusion, cesarean delivery presents unique challenges for healthcare providers, particularly nurses. By prioritizing key assessment findings such as vital signs, uterine assessment, and incision site examination, nurses can play a crucial role in the early identification of complications. Implementing evidence-based practices further enhances the quality of care provided to mothers and their newborns. We encourage healthcare professionals to engage in discussions, share experiences, and stay informed about the best practices in managing cesarean deliveries.
If you found this article helpful, please leave a comment below or share it with your colleagues. For more informative articles, feel free to explore our website.
Thank you for reading, and we look forward to seeing you again!
ncG1vNJzZmivp6x7rLHLpbCmp5%2Bnsm%2BvzqZmm6efqMFuxc6uqWarlaR8pLHSmqmemZ5isaa4yK%2Bcq7FdrLWqr8dmmKyrlajArrHNrWSfoZ6Ztq%2BzjKyfqK2cmXq1tMRmpa6qo5p6sb7IqKmirJmvsm61xWefraWc