When it comes to skin ulcers, understanding the differences between arterial and venous ulcers is crucial for effective diagnosis and treatment. These two types of ulcers arise from different underlying conditions and have distinct characteristics. In this comprehensive guide, we will delve into the causes, symptoms, treatment options, and preventive measures for both arterial and venous ulcers, providing you with the necessary information to make informed decisions about your health.
Arterial ulcers are typically caused by poor blood circulation due to arterial blockages, whereas venous ulcers result from improper blood flow in the veins. Recognizing these differences can significantly impact the management and healing of these wounds. By the end of this article, you will have a clearer understanding of these conditions and how to address them effectively.
We will cover a variety of topics, including the anatomy of the circulatory system, risk factors for each type of ulcer, and the latest treatment approaches. Whether you are a healthcare professional seeking to enhance your knowledge or someone affected by these ulcers, this guide aims to equip you with valuable insights.
Table of Contents
Understanding Arterial and Venous Ulcers
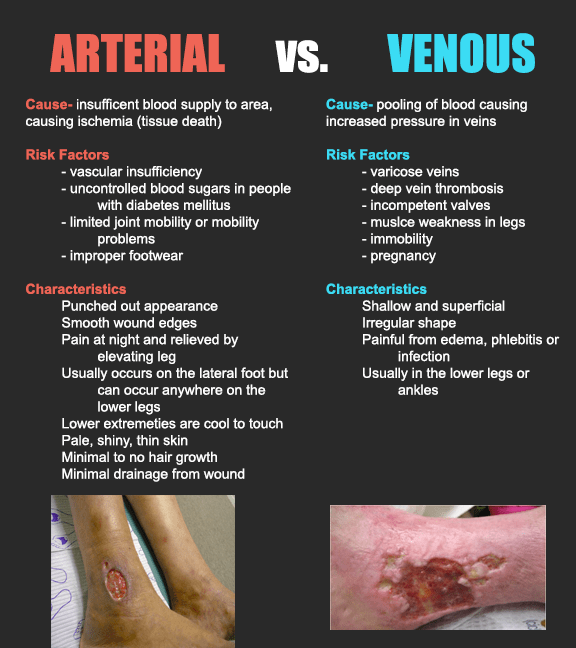
Arterial and venous ulcers represent two distinct types of chronic wounds that occur primarily due to circulatory issues. Arterial ulcers, often located on the feet and toes, are caused by insufficient blood flow resulting from conditions such as peripheral artery disease (PAD). On the other hand, venous ulcers typically occur in the lower legs and are linked to venous insufficiency, where veins fail to return blood to the heart efficiently.
Key Differences Between Arterial and Venous Ulcers
- Location: Arterial ulcers usually appear on the feet and toes, while venous ulcers are more common around the ankles.
- Appearance: Arterial ulcers often have a "punched-out" appearance with well-defined edges, whereas venous ulcers typically have irregular borders and may be accompanied by surrounding skin discoloration.
- Pain Levels: Arterial ulcers tend to be more painful, especially when the legs are elevated, while venous ulcers may cause aching or heaviness in the legs.
Causes of Arterial and Venous Ulcers
The underlying causes of arterial and venous ulcers are primarily linked to blood circulation issues. Understanding these causes helps in prevention and treatment.
Causes of Arterial Ulcers
- Peripheral Artery Disease (PAD): A condition where arteries narrow, reducing blood flow to the limbs.
- Diabetes: High blood sugar levels can damage blood vessels, increasing the risk of ulcers.
- Smoking: Tobacco use contributes to vascular diseases, leading to arterial ulcers.
Causes of Venous Ulcers
- Venous Insufficiency: A condition where veins cannot pump blood back to the heart effectively.
- Deep Vein Thrombosis (DVT): A blood clot in a deep vein can lead to chronic venous insufficiency.
- Obesity: Excess weight puts additional pressure on veins, increasing the risk of venous ulcers.
Symptoms of Arterial and Venous Ulcers
Recognizing the symptoms of both arterial and venous ulcers is essential for timely intervention.
Symptoms of Arterial Ulcers
- Pain: Severe pain in the affected area, especially when the leg is elevated.
- Skin Changes: Shiny, thin skin; hair loss on the legs; and cool skin temperature.
- Ulcer Characteristics: Deep, well-defined edges, often with a necrotic base.
Symptoms of Venous Ulcers
- Leg Swelling: Swelling around the ankles and lower legs.
- Skin Changes: Brown discoloration and thickening of the skin.
- Ulcer Characteristics: Shallow, irregularly shaped ulcers with a red or yellow base.
Diagnosis of Arterial and Venous Ulcers
Accurate diagnosis is vital for determining the appropriate treatment for both types of ulcers.
- Medical History: A thorough review of the patient's medical history, including risk factors.
- Physical Examination: Inspecting the ulcer, assessing blood flow, and checking for signs of infection.
- Imaging Tests: Doppler ultrasound and angiography may be used to evaluate blood flow.
Treatment Options for Arterial Ulcers
Treatment for arterial ulcers focuses on improving blood flow and wound care.
- Revascularization: Surgical procedures to restore blood flow, such as angioplasty or bypass surgery.
- Wound Care: Regular cleaning and dressing of the ulcer to prevent infection.
- Medication: Prescribing medications to manage pain and improve circulation.
Treatment Options for Venous Ulcers
Venous ulcers require a different approach, primarily focused on improving venous circulation.
- Compression Therapy: Using compression bandages or stockings to reduce swelling and improve blood flow.
- Wound Care: Proper cleaning and dressing of the ulcer to promote healing.
- Medications: Topical treatments and systemic medications to manage symptoms and prevent infection.
Preventive Measures for Ulcers
Preventing both arterial and venous ulcers involves addressing the underlying risk factors.
- Healthy Lifestyle: Maintaining a balanced diet, regular exercise, and avoiding smoking.
- Weight Management: Keeping a healthy weight to reduce pressure on veins and arteries.
- Regular Check-ups: Monitoring for conditions like diabetes and hypertension.
Conclusion
In summary, understanding the differences between arterial and venous ulcers is vital for effective treatment and management. By recognizing the symptoms, causes, and treatment options, individuals can take proactive steps toward prevention and healing. If you or someone you know is experiencing symptoms of ulcers, consult a healthcare professional for proper diagnosis and treatment.
We encourage our readers to leave comments or share this article with those who might benefit from the information. For more health-related articles, explore our site and stay informed about your health.
ncG1vNJzZmivp6x7rLHLpbCmp5%2Bnsm%2BvzqZmp52nqLCwvsRubGiZoqmys7XApWSvq12rsq%2B71KxkrqSTmr%2B0esetpKU%3D