Bob Marley, a name synonymous with reggae music, remains an iconic figure in the music industry. However, beyond his timeless melodies and impactful lyrics, he is also remembered for a significant health battle that ended his life prematurely. Marley was diagnosed with malignant melanoma, a severe form of skin cancer, which ultimately led to his untimely passing at the age of 36. This article delves into the details of malignant melanoma, exploring its causes, symptoms, and treatments, while highlighting how Bob Marley's experience brought attention to this aggressive disease. We aim to shed light on the importance of awareness and early detection, particularly for those with darker skin tones, who may be under the misconception that they are less susceptible to skin cancers.
Malignant melanoma is a type of cancer that originates in the melanocytes, the cells responsible for producing melanin, the pigment that colors our skin. It is notorious for its ability to spread rapidly to other parts of the body, making it one of the most dangerous forms of skin cancer. Despite its severity, early detection and treatment can significantly improve survival rates. Bob Marley's personal battle with malignant melanoma highlighted the fact that this disease does not discriminate, affecting individuals regardless of their race or skin color. His diagnosis came as a shock to many, challenging the prevailing notion that darker-skinned individuals are immune to skin cancer.
In this comprehensive exploration, we will discuss Bob Marley's life and career, his experience with malignant melanoma, and the broader implications of the disease. We will also provide insights into the prevention, diagnosis, and treatment of malignant melanoma, emphasizing the importance of vigilance and regular skin checks. By examining Marley's journey, we hope to inspire a greater understanding of malignant melanoma and promote proactive health measures to combat this formidable disease.
Table of Contents
Bob Marley's Biography
Bob Marley, born on February 6, 1945, in Nine Mile, Jamaica, was a legendary reggae musician whose influence transcended music. His unique blend of reggae, ska, and rocksteady, infused with socially conscious lyrics, made him a global icon. Marley's music advocated for peace, love, and unity, resonating with audiences worldwide.
Marley's journey began in the rural village of Nine Mile, where he was raised by his mother, Cedella Booker. His father, Norval Marley, was a white Jamaican of English descent, while his mother was of Afro-Jamaican heritage. This mixed heritage influenced Marley's identity and music, allowing him to connect with diverse audiences.
In the early 1960s, Bob Marley formed the Wailers with Peter Tosh and Bunny Wailer. The group achieved local success in Jamaica before gaining international recognition in the 1970s. Marley's album "Catch a Fire" catapulted him to fame, followed by iconic albums like "Rastaman Vibration," "Exodus," and "Legend." His music was not only celebrated for its catchy rhythms but also for its powerful messages addressing social justice, spirituality, and human rights.
Marley's influence extended beyond music; he became a symbol of resistance against oppression and a voice for the marginalized. His Rastafarian beliefs, rooted in African identity and spirituality, were integral to his persona. Marley's dreadlocks, a hallmark of his image, were a manifestation of his faith and commitment to cultural authenticity.
| Personal Details | Information |
|---|---|
| Full Name | Robert Nesta Marley |
| Date of Birth | February 6, 1945 |
| Place of Birth | Nine Mile, Saint Ann Parish, Jamaica |
| Date of Death | May 11, 1981 |
| Occupation | Musician, Singer, Songwriter |
| Genres | Reggae, Ska, Rocksteady |
| Famous Albums | "Catch a Fire," "Rastaman Vibration," "Exodus," "Legend" |
Understanding Malignant Melanoma
Malignant melanoma is a type of skin cancer that arises from the melanocytes, the cells responsible for producing the pigment melanin, which gives skin its color. Unlike other forms of skin cancer, melanoma is particularly aggressive and can metastasize to other parts of the body if not detected early. It is considered the deadliest form of skin cancer, accounting for a significant number of skin cancer-related deaths worldwide.
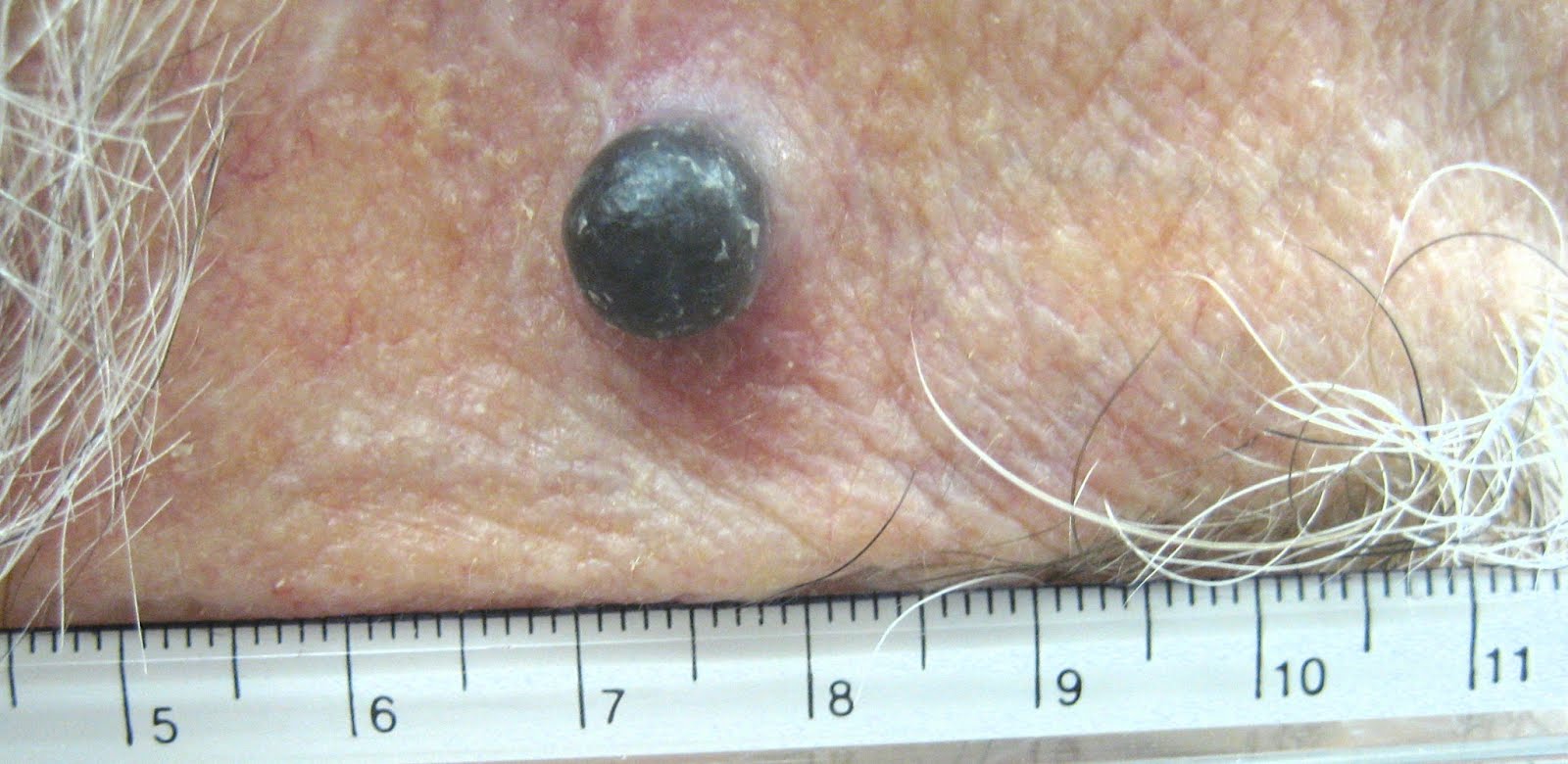
Melanoma can develop anywhere on the skin, but it is most commonly found in areas exposed to the sun, such as the face, arms, and legs. However, it can also occur in less exposed areas, such as the soles of the feet, palms, and under the nails. This is particularly relevant for individuals with darker skin, as melanomas in these areas may go unnoticed until they have progressed to a more advanced stage.
The primary cause of melanoma is ultraviolet (UV) radiation from the sun or tanning beds, which can damage the DNA in skin cells. However, genetic factors, family history, and certain hereditary conditions can also increase an individual's risk of developing melanoma. It's important to note that while sun exposure is a significant risk factor, melanomas can develop in areas not exposed to the sun, indicating that other factors are also at play.
Recognizing the early signs of melanoma is crucial for effective treatment. The ABCDE rule is a helpful guide for identifying suspicious moles or skin changes:
- A - Asymmetry: One half of the mole does not match the other.
- B - Border: The edges are irregular, ragged, or blurred.
- C - Color: The color is not uniform and may include shades of brown, black, red, white, or blue.
- D - Diameter: The mole is larger than 6 millimeters (about the size of a pencil eraser).
- E - Evolving: The mole is changing in size, shape, or color.
Early detection and treatment of melanoma can significantly improve survival rates. If caught early, melanoma can often be treated successfully with surgery to remove the tumor. However, if it has spread to other parts of the body, more advanced treatments such as immunotherapy, targeted therapy, or chemotherapy may be required.
Risk Factors and Causes
The development of malignant melanoma is influenced by a combination of genetic, environmental, and lifestyle factors. Understanding these risk factors can help individuals take preventive measures to reduce their chances of developing this aggressive form of skin cancer.
One of the primary risk factors for melanoma is prolonged exposure to ultraviolet (UV) radiation, which can damage the DNA in skin cells and lead to cancerous changes. UV radiation is primarily obtained from the sun, but artificial sources such as tanning beds also pose a significant risk. People who spend a lot of time outdoors without adequate sun protection or those who frequently use tanning beds are at an increased risk of developing melanoma.
Fair-skinned individuals, particularly those with light hair and eye color, are more susceptible to UV damage and therefore have a higher risk of melanoma. However, it's critical to note that melanoma can affect people of all skin tones, including those with darker skin. In these cases, melanoma often develops in less exposed areas, such as the palms, soles, and under the nails, making early detection more challenging.
Genetic factors also play a significant role in melanoma risk. Individuals with a family history of melanoma are at an increased risk, as are those with certain genetic mutations. In particular, mutations in the CDKN2A and BRAF genes have been associated with an increased risk of melanoma. Additionally, individuals with a history of atypical moles or dysplastic nevi, which are unusual-looking moles that may resemble melanoma, are at a higher risk.
Other factors that can increase the risk of melanoma include:
- Previous Skin Cancer: A history of melanoma or other skin cancers increases the risk of developing melanoma.
- Suppressed Immune System: Individuals with weakened immune systems, such as organ transplant recipients or those with HIV/AIDS, are at a higher risk.
- Age and Gender: Melanoma is more common in older adults, but it can occur at any age. It is also more prevalent in men than women, although this varies by age group.
- Geographic Location: People living closer to the equator or at higher altitudes are exposed to more intense UV radiation and are at a greater risk.
Understanding these risk factors can empower individuals to take proactive steps in protecting their skin and monitoring for any changes. Regular skin checks, sun protection measures, and awareness of personal risk factors are essential in reducing the risk of melanoma.
Symptoms and Early Detection
Early detection of malignant melanoma is crucial for successful treatment and improved survival rates. Recognizing the symptoms and understanding how to identify potential melanoma can make a significant difference in outcomes.
The most common symptom of melanoma is a change in an existing mole or the appearance of a new, unusual-looking mole on the skin. Melanomas can vary in appearance, but they often have distinct characteristics that set them apart from benign moles. The ABCDE rule is a helpful guideline for identifying suspicious moles:
- A - Asymmetry: One half of the mole does not match the other in shape or size.
- B - Border: Melanomas often have irregular, scalloped, or poorly defined borders.
- C - Color: The color of a melanoma may not be uniform and can include shades of brown, black, red, white, or blue.
- D - Diameter: Melanomas are usually larger than 6 millimeters (about the size of a pencil eraser), but they can be smaller when first detected.
- E - Evolving: Any change in size, shape, color, or elevation of a mole, or any new symptom such as bleeding, itching, or crusting, should be evaluated by a healthcare professional.
In addition to changes in moles, other symptoms of melanoma can include:
- The appearance of a new, unusual growth or sore that does not heal.
- A change in sensation, such as itchiness, tenderness, or pain in a mole or skin lesion.
- The spread of pigment from the border of a mole into surrounding skin.
Regular self-examinations of the skin can help detect early signs of melanoma. It's important to become familiar with the pattern of moles, freckles, and other marks on your skin so you can notice any changes. Performing a monthly skin check using mirrors or enlisting the help of a partner can aid in examining difficult-to-see areas.
If you notice any changes or new growths on your skin, it's essential to consult a dermatologist or healthcare provider promptly. Early detection and treatment are critical for improving the chances of a successful outcome. Dermatologists may use a dermatoscope, a specialized tool for examining skin lesions, to assess suspicious moles. If necessary, a biopsy may be performed to confirm a diagnosis of melanoma.
Diagnosis and Staging
Diagnosing malignant melanoma involves a thorough examination of the skin and, if necessary, a biopsy to confirm the presence of cancerous cells. Once melanoma is diagnosed, staging is an essential step in determining the extent of the cancer and planning the appropriate treatment approach.
The diagnostic process typically begins with a physical examination by a dermatologist, who will assess any suspicious moles or skin changes using visual inspection and tools like a dermatoscope. If a lesion is deemed suspicious, a biopsy is performed to obtain a sample of the tissue for laboratory analysis. There are several types of biopsies used in diagnosing melanoma:
- Excisional Biopsy: The entire mole or lesion is removed along with a margin of surrounding healthy skin.
- Incisional Biopsy: A portion of the mole or lesion is removed for examination.
- Punch Biopsy: A circular tool is used to remove a small, cylindrical sample of skin tissue.
- Shave Biopsy: The top layers of the skin are shaved off for analysis.
Once melanoma is confirmed, staging is performed to determine the extent of cancer. Staging is based on the thickness of the tumor, the involvement of lymph nodes, and whether the cancer has spread to other parts of the body (metastasis). The American Joint Committee on Cancer (AJCC) staging system is commonly used and includes the following stages:
- Stage 0 (In Situ): The cancer is confined to the epidermis (top layer of skin) and has not spread.
- Stage I: The cancer is small (less than 2mm thick) and has not spread to lymph nodes.
- Stage II: The cancer is thicker (more than 2mm) but has not spread to lymph nodes or distant sites.
- Stage III: The cancer has spread to nearby lymph nodes or tissues.
- Stage IV: The cancer has spread to distant lymph nodes or organs, indicating advanced melanoma.
Staging is crucial for determining the most appropriate treatment plan and assessing the prognosis. Early-stage melanomas (stages 0 and I) are often treated with surgical removal of the tumor, while more advanced stages may require additional treatments such as immunotherapy, targeted therapy, or chemotherapy.
Advances in diagnostic tools and staging techniques have improved the accuracy of melanoma assessment, allowing for more personalized treatment approaches. Genetic testing and molecular profiling of tumors may also be used to identify specific mutations and tailor treatments accordingly.
Treatment Options
The treatment of malignant melanoma depends on the stage of the cancer, the location of the tumor, and the overall health of the patient. Early-stage melanomas can often be treated successfully with surgical intervention, while more advanced stages may require a combination of treatments to address the spread of the disease.
Surgery is the primary treatment for early-stage melanoma. The goal is to remove the tumor along with a margin of healthy tissue to ensure complete excision. The extent of surgery depends on the thickness and location of the melanoma. In some cases, a sentinel lymph node biopsy may be performed to assess the involvement of nearby lymph nodes and determine if further treatment is needed.
For melanomas that have spread beyond the original site or are more advanced, additional treatment options may be considered:
- Immunotherapy: This treatment uses the body's immune system to target and destroy cancer cells. Immune checkpoint inhibitors, such as pembrolizumab and nivolumab, have shown promise in treating advanced melanoma by enhancing the immune response against cancer cells.
- Targeted Therapy: This approach involves using drugs that target specific genetic mutations or proteins involved in melanoma growth. BRAF and MEK inhibitors, such as vemurafenib and cobimetinib, are commonly used for melanomas with BRAF mutations.
- Chemotherapy: Although less commonly used for melanoma, chemotherapy may be considered for advanced cases that do not respond to other treatments. Drugs like dacarbazine and temozolomide are used to kill cancer cells or slow their growth.
- Radiation Therapy: This treatment uses high-energy rays to target and destroy cancer cells. It may be used to treat melanoma that has spread to other parts of the body or to alleviate symptoms in advanced cases.
In addition to conventional treatments, clinical trials and experimental therapies may be considered for patients with advanced melanoma. These trials assess the effectiveness of new drugs or treatment combinations and provide access to cutting-edge therapies.
Supportive care and palliative treatments are also important components of melanoma management, particularly for advanced cases. These approaches focus on improving quality of life, managing symptoms, and providing emotional and psychological support to patients and their families.
It's essential for patients to work closely with a multidisciplinary team of healthcare professionals, including dermatologists, oncologists, and surgeons, to develop a personalized treatment plan. Advances in melanoma research continue to expand the range of treatment options, offering hope for improved outcomes and survival rates.
Bob Marley's Battle with Malignant Melanoma
Bob Marley's battle with malignant melanoma is a poignant reminder of the indiscriminate nature of this aggressive disease. Despite his global fame and influence, Marley faced a significant health challenge that ultimately ended his life. His diagnosis and subsequent journey with melanoma brought attention to the importance of awareness, early detection, and the unique challenges faced by individuals with darker skin tones.
Marley's melanoma was first discovered in 1977 when he sustained an injury to his toe during a soccer match. What initially appeared to be a simple bruise turned out to be something far more serious. A biopsy revealed that the lesion on his toe was a malignant melanoma. Despite the diagnosis, Marley chose to continue his music career and adhere to his Rastafarian beliefs, which influenced his approach to treatment.
At the time, Marley opted for a conservative approach to treatment, choosing not to undergo amputation of the toe as recommended by his doctors. Instead, he underwent a surgical procedure to remove the cancerous tissue, followed by skin grafting. While Marley continued to perform and tour, the melanoma persisted and eventually spread to other parts of his body.
By the time Marley sought further medical intervention, the melanoma had metastasized to his brain, lungs, and liver, significantly impacting his health. Despite his declining condition, Marley remained committed to his music and message, performing one of his final concerts in Pittsburgh in September 1980.
Bob Marley's battle with melanoma ended on May 11, 1981, when he passed away at the age of 36. His death was a profound loss to the music world, but it also served as a wake-up call about the realities of melanoma. Marley's experience highlighted the need for awareness and vigilance, particularly for individuals who may not consider themselves at risk for skin cancer.
Marley's legacy extends beyond his music; his journey with melanoma has inspired conversations about skin cancer prevention, early detection, and the importance of addressing health disparities. His story underscores the need for regular skin checks, sun protection, and education about melanoma risk factors, regardless of skin color.
The Impact of Bob Marley's Diagnosis
Bob Marley's diagnosis of malignant melanoma had a profound impact on his fans, the medical community, and the broader understanding of skin cancer. His experience brought attention to the fact that melanoma can affect anyone, regardless of race or skin color, challenging prevailing misconceptions and emphasizing the importance of awareness and early detection.
Marley's diagnosis served as a wake-up call for many individuals who may have believed that darker skin provided immunity against skin cancer. His case highlighted the reality that melanoma can occur in less exposed areas, such as the soles of the feet and under the nails, which are often overlooked during skin checks. This revelation prompted increased awareness of the need for comprehensive skin examinations, particularly for people of African, Asian, and Hispanic descent.
The impact of Marley's diagnosis extended beyond individual awareness; it also influenced the medical community's approach to melanoma. Healthcare professionals recognized the importance of educating patients about the risk factors for melanoma, regardless of skin tone, and the need for regular skin examinations. Marley's case underscored the importance of cultural sensitivity and understanding in healthcare, particularly when addressing health disparities and promoting preventive measures.
In addition to raising awareness, Bob Marley's experience with melanoma contributed to advancements in melanoma research and treatment. His case highlighted the need for more effective therapies and prompted further investigation into the genetic and environmental factors contributing to melanoma in diverse populations. Researchers and clinicians have since made significant strides in understanding melanoma, leading to the development of targeted therapies and immunotherapies that have improved outcomes for many patients.
Marley's legacy continues to inspire advocacy efforts aimed at promoting skin cancer awareness, prevention, and early detection. Organizations and campaigns dedicated to melanoma education often reference Marley's story as a powerful example of the importance of vigilance and proactive health measures. His influence has helped dismantle stereotypes and encouraged individuals of all backgrounds to take their skin health seriously.
Ultimately, Bob Marley's diagnosis of malignant melanoma serves as a reminder that skin cancer does not discriminate. His journey has left an indelible mark on the fight against melanoma, inspiring greater understanding, compassion, and action to address this formidable disease.
Prevention and Awareness
Preventing malignant melanoma involves a combination of protective measures, awareness of risk factors, and proactive skin health practices. While melanoma can be aggressive and challenging to treat, early detection and prevention strategies can significantly reduce the risk of developing this form of skin cancer.
One of the most effective ways to prevent melanoma is to minimize exposure to ultraviolet (UV) radiation, the primary environmental risk factor for skin cancer. UV radiation is emitted by the sun and artificial sources such as tanning beds. Taking the following precautions can help protect the skin from harmful UV rays:
- Seek Shade: Limit time spent in direct sunlight, especially during peak hours when UV rays are strongest (10 a.m. to 4 p.m.).
- Wear Protective Clothing: Cover the skin with long-sleeved shirts, pants, wide-brimmed hats, and sunglasses to shield against UV rays.
- Use Sunscreen: Apply a broad-spectrum sunscreen with an SPF of at least 30 to all exposed skin, and reapply every two hours or after swimming or sweating.
- Avoid Tanning Beds: Refrain from using tanning beds and artificial tanning devices, which emit UV radiation and increase the risk of melanoma.
In addition to sun protection, regular skin checks are essential for early detection of melanoma. Conducting monthly self-examinations allows individuals to become familiar with their skin and identify any changes or new growths. A full-body skin examination by a dermatologist is recommended annually or more frequently for individuals at higher risk.
Understanding personal risk factors for melanoma can also aid in prevention. Individuals with a family history of melanoma, a history of atypical moles, fair skin, or a history of sunburns should be particularly vigilant in monitoring their skin and taking preventive measures.
Education and awareness campaigns play a crucial role in promoting melanoma prevention and early detection. Public health initiatives, community outreach programs, and advocacy organizations work to raise awareness about the importance of sun protection, regular skin checks, and recognizing the signs of melanoma. These efforts aim to empower individuals with the knowledge and tools needed to reduce their risk and improve their skin health.
Ultimately, preventing melanoma requires a multifaceted approach that combines lifestyle changes, education, and regular monitoring. By prioritizing skin health and staying informed about risk factors, individuals can take proactive steps to protect themselves and reduce their risk of developing malignant melanoma.
The Role of Family History
Family history plays a significant role in the risk of developing malignant melanoma. Understanding the genetic and hereditary factors associated with melanoma can help individuals assess their risk and take appropriate preventive measures.
Research has shown that individuals with a family history of melanoma have a higher risk of developing the disease themselves. This increased risk is attributed to shared genetic mutations and hereditary factors that may predispose family members to melanoma. In particular, mutations in genes such as CDKN2A and BRAF have been linked to an increased risk of melanoma.
The CDKN2A gene provides instructions for making proteins that regulate cell growth and division. Mutations in this gene can lead to uncontrolled cell growth, increasing the likelihood of melanoma development. Similarly, mutations in the BRAF gene, which is involved in cell signaling pathways, can contribute to the growth and spread of melanoma cells.
Individuals with a family history of melanoma should be particularly vigilant in monitoring their skin and taking preventive measures. Regular skin examinations, both self-exams and professional evaluations, are essential for early detection. It is also important for these individuals to be aware of the ABCDE rule for identifying suspicious moles and to seek medical evaluation if any changes are observed.
Genetic counseling and testing may be recommended for individuals with a strong family history of melanoma. Genetic testing can identify specific mutations that may indicate an increased risk of melanoma and other cancers. This information can help guide personalized prevention strategies and inform decisions about screening and monitoring.
In addition to genetic factors, environmental and lifestyle factors can also influence melanoma risk within families. Shared behaviors, such as sun exposure habits and the use of sun protection, can contribute to the risk of melanoma. Educating family members about the importance of sun protection and skin health can help reduce the overall risk within families.
Overall, understanding the role of family history in melanoma risk emphasizes the importance of awareness, education, and proactive health measures. By recognizing their genetic predisposition and taking preventive steps, individuals with a family history of melanoma can reduce their risk and improve their chances of early detection and successful treatment.
Skin Cancer Screening and Checks
Regular screening and skin checks are essential components of skin cancer prevention and early detection. Identifying suspicious moles or lesions at an early stage can significantly improve the chances of successful treatment and survival. Understanding the importance of screening and how to perform effective skin checks can empower individuals to take control of their skin health.
Skin cancer screening involves a thorough examination of the skin to identify any unusual moles, growths, or lesions that may be indicative of skin cancer. Dermatologists and healthcare professionals use a combination of visual inspection and diagnostic tools to assess the skin and identify potential concerns.
During a professional skin examination, a dermatologist will carefully examine the entire skin surface, paying close attention to areas commonly affected by skin cancer, such as the face, neck, arms, and legs. They may use a dermatoscope, a specialized magnifying tool, to examine moles and lesions in greater detail. This tool allows for the evaluation of structures beneath the skin's surface, aiding in the differentiation between benign and malignant lesions.
In addition to professional screenings, regular self-examinations are a crucial part of skin cancer prevention. Performing a monthly self-check allows individuals to become familiar with their skin's normal appearance and detect any changes or new growths. The following steps can guide an effective self-examination:
- Find a Well-Lit Area: Use a full-length mirror and a hand-held mirror to examine hard-to-see areas.
- Check All Areas: Examine the entire body, including the scalp, face, neck, arms, legs, chest, back, and buttocks. Don't forget less exposed areas like the soles of the feet, between the toes, and under the nails.
- Use the ABCDE Rule: Pay attention to moles or lesions that exhibit asymmetry, irregular borders, multiple colors, large diameter, or any changes over time.
- Document Changes: Take note of any new or changing moles, and consider taking photographs to track changes over time.
If any suspicious moles or lesions are identified during a self-examination, it is important to schedule an appointment with a dermatologist for further evaluation. Early intervention is key to addressing potential skin cancer and preventing further progression.
Public health campaigns and educational initiatives continue to emphasize the importance of regular skin checks and screenings. By prioritizing skin health and awareness, individuals can reduce their risk of developing skin cancer and improve their chances of early detection and successful treatment.
Advancements in Research and Treatment
In recent years, significant advancements in melanoma research and treatment have transformed the landscape of care for this aggressive form of skin cancer. These developments have improved our understanding of melanoma biology, genetics, and treatment options, offering hope for better outcomes and survival rates.
One of the most notable advancements in melanoma treatment is the development of targeted therapies. These therapies focus on specific genetic mutations or molecular pathways that drive melanoma growth. For example, BRAF inhibitors, such as vemurafenib and dabrafenib, target the BRAF mutation found in approximately 50% of melanomas. These drugs have shown remarkable efficacy in shrinking tumors and prolonging survival in patients with BRAF-mutant melanoma.
In addition to targeted therapies, immunotherapy has emerged as a groundbreaking approach in melanoma treatment. Immune checkpoint inhibitors, such as pembrolizumab and nivolumab, work by enhancing the body's immune response to cancer cells. These drugs have demonstrated significant success in treating advanced melanoma, leading to durable responses and long-term survival in some patients.
Advances in precision medicine have also contributed to improved melanoma treatment. Molecular profiling and genetic testing allow for the identification of specific mutations and biomarkers in individual tumors. This information enables healthcare providers to tailor treatments to each patient's unique genetic profile, optimizing therapy effectiveness and minimizing side effects.
Furthermore, ongoing research continues to explore novel therapeutic approaches and combination therapies for melanoma. Clinical trials are investigating new drugs, treatment combinations, and innovative strategies to overcome resistance and improve patient outcomes. These efforts hold promise for expanding the range of treatment options available to melanoma patients.
In addition to treatment advancements, research in melanoma prevention and early detection has also made significant strides. Public health initiatives and educational campaigns have increased awareness of melanoma risk factors, sun protection, and the importance of regular skin checks. The development of advanced imaging techniques, such as total body photography and dermoscopy, has improved the accuracy of melanoma detection and monitoring.
The impact of these advancements is reflected in improved survival rates and quality of life for many melanoma patients. While challenges remain, the progress made in melanoma research and treatment offers hope for continued advancements and breakthroughs in the fight against this formidable disease.
Living with Malignant Melanoma
Living with a diagnosis of malignant melanoma can be challenging, both physically and emotionally. However, with the right support, resources, and proactive measures, individuals can navigate the journey and maintain a high quality of life.
One of the key aspects of living with melanoma is ongoing medical monitoring and follow-up care. Regular check-ups with healthcare providers, including dermatologists and oncologists, are essential for monitoring the condition and detecting any potential recurrences or complications. Follow-up care may include imaging tests, blood work, and skin examinations to assess treatment response and overall health.
Support from healthcare professionals and a multidisciplinary team can provide individuals with the guidance and resources needed to manage their condition effectively. This team may include medical specialists, nurses, counselors, and support group facilitators who can address the physical, emotional, and psychological aspects of living with melanoma.
In addition to medical care, lifestyle modifications and self-care practices play a crucial role in managing melanoma. Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and stress management, can support overall well-being and enhance the body's ability to cope with the challenges of cancer treatment.
Emotional support and mental health care are equally important for individuals living with melanoma. A cancer diagnosis can bring about a range of emotions, including fear, anxiety, and uncertainty. Seeking support from mental health professionals, support groups, or counseling services can provide individuals with the tools to cope with these emotions and navigate the emotional impact of melanoma.
Education and empowerment are vital components of living with melanoma. Staying informed about the condition, treatment options, and available resources can empower individuals to make informed decisions about their care and take an active role in their treatment journey. Engaging with advocacy organizations, participating in educational programs, and connecting with others who have experienced melanoma can provide valuable insights and support.
Ultimately, living with malignant melanoma requires a comprehensive approach that addresses the physical, emotional, and social aspects of the disease. By prioritizing health, seeking support, and staying informed, individuals can navigate the challenges of melanoma and maintain a meaningful and fulfilling life.
Global Perspective on Malignant Melanoma
Malignant melanoma is a global health concern, with varying incidence rates and challenges across different regions and populations. Understanding the global perspective on melanoma provides valuable insights into the factors influencing its prevalence, prevention, and treatment worldwide.
While melanoma is most prevalent in regions with high UV exposure, such as Australia, New Zealand, and parts of North America and Europe, it affects populations worldwide. The incidence of melanoma has been rising in many countries, attributed to factors such as increased sun exposure, changing behaviors, and improved detection methods.
In countries with predominantly fair-skinned populations, such as Australia and New Zealand, melanoma is a leading cause of cancer-related morbidity and mortality. Public health campaigns in these regions have focused on sun safety, promoting protective behaviors, and raising awareness about the importance of regular skin checks. These efforts have contributed to improved early detection and reduced mortality rates in some areas.
In contrast, regions with diverse populations and varying skin tones face unique challenges in addressing melanoma. In many African, Asian, and Hispanic communities, melanoma awareness is often limited, and misconceptions about skin cancer risk persist. Melanomas in individuals with darker skin are more likely to occur in less exposed areas, leading to delayed diagnosis and poorer outcomes. Efforts are needed to improve education, access to care, and cultural sensitivity in addressing melanoma in these populations.
Global collaborations and research initiatives play a crucial role in advancing our understanding of melanoma and developing effective prevention and treatment strategies. International organizations, such as the World Health Organization (WHO) and the International Agency for Research on Cancer (IARC), work to promote awareness, research, and evidence-based interventions to combat melanoma worldwide.
Addressing melanoma on a global scale requires a multifaceted approach that considers regional differences, cultural factors, and healthcare disparities. By promoting education, improving access to care, and fostering international collaboration, the global community can work towards reducing the burden of malignant melanoma and improving outcomes for individuals affected by this aggressive disease.
Frequently Asked Questions
- What is malignant melanoma?
- What are the risk factors for melanoma?
- How can I prevent melanoma?
- What is the ABCDE rule for identifying melanoma?
- How is melanoma treated?
- What impact did Bob Marley have on melanoma awareness?
Malignant melanoma is a type of skin cancer that originates in the melanocytes, the cells responsible for producing melanin, the pigment that colors our skin. It is known for its aggressive nature and ability to spread rapidly to other parts of the body.
Risk factors for melanoma include prolonged exposure to UV radiation, fair skin, family history of melanoma, presence of atypical moles, and a weakened immune system. People with darker skin can also develop melanoma, often in less-exposed areas.
Preventing melanoma involves minimizing UV exposure, using sunscreen, wearing protective clothing, avoiding tanning beds, and performing regular skin checks. Being aware of personal risk factors and practicing sun safety are key preventive measures.
The ABCDE rule is a guideline for identifying suspicious moles: Asymmetry, Border irregularity, Color variation, Diameter larger than 6mm, and Evolving changes in size, shape, or color. Any changes should be evaluated by a healthcare professional.
Treatment for melanoma depends on the stage and may include surgery, immunotherapy, targeted therapy, chemotherapy, and radiation therapy. Early-stage melanomas are often treated with surgical removal, while advanced cases may require additional therapies.
Bob Marley's battle with malignant melanoma brought attention to the disease and challenged misconceptions about skin cancer risk in individuals with darker skin. His legacy continues to inspire awareness, education, and advocacy efforts worldwide.
Conclusion
Malignant melanoma, a formidable form of skin cancer, poses significant challenges but also opportunities for prevention, early detection, and treatment. Bob Marley's journey with melanoma serves as a powerful reminder of the disease's indiscriminate nature and the importance of awareness and vigilance. Through continued research, education, and global collaboration, we can work towards reducing the burden of melanoma and improving outcomes for individuals affected by this aggressive disease. By prioritizing skin health and taking proactive measures, we can honor Marley's legacy and contribute to a future where melanoma is detected early and treated effectively.
ncG1vNJzZmivp6x7rLHLpbCmp5%2Bnsm%2BvzqZmpJ2cocZussinoKygX6KurbXGp5inrF2isq2tzaikmmWSpK9uucCro56xXp3Brrg%3D